Recently my 11-year-old twins were asking me the difference between accuracy and precision in scientific measurement. At first, excited by the prospect that they were inquiring about my work, I launched into a dissertation on the topic and quickly came to realize it was for me to complete their fifth-grade homework assignment. Nonetheless after 10 minutes of purposeful torture explaining to them the difference, I got nothing but the blank look of two kids who realized they should have asked Alexa 9.5 minutes ago.
While my kids are still recovering from this interaction, it did get me thinking about accuracy and precision in surgical robotics and the nature by which we achieve and guide them both. More importantly, it got me thinking philosophically about whether we should be designing systems that autonomously control both for the best outcome of the patient.
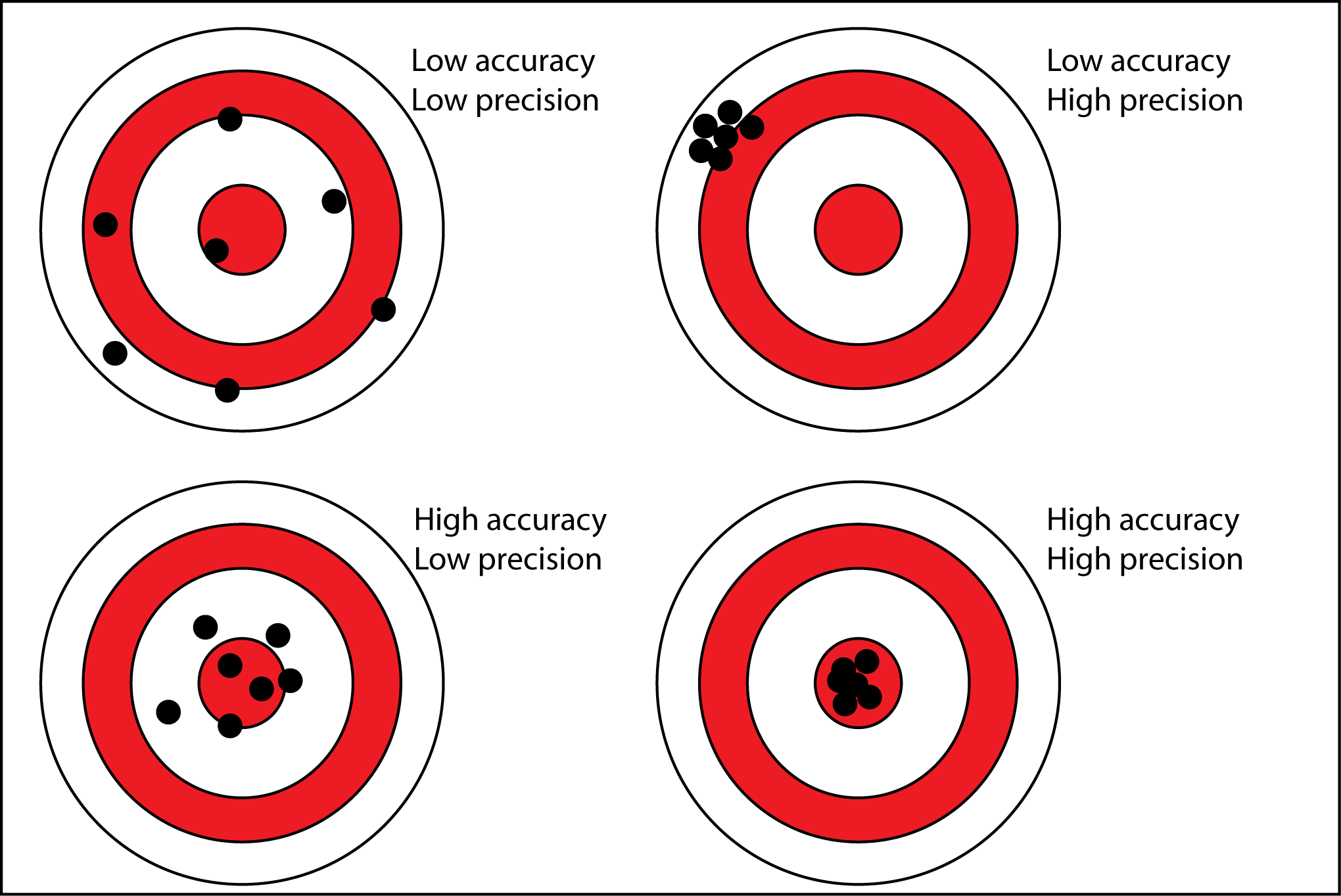
Let’s take for a second a robotic guidance system like the Mazor X for spine surgery or the Mako System for knee and hip replacement. Surgeons require, as they should, those systems be accurate to their plan and precise while using them. As seen on the upper left of Figure 1, we cannot have a system that is trying to reach the same target each time but at each trajectory finds a new location.
Want to learn more?
Safety and wellbeing in surgical robotics
This lack of precision is a non-starter and its lack of accuracy to the planned trajectory is equally unacceptable for the safety and wellbeing of the patient. There is a massive amount of complex cross functional engineering that is needed to make these small movements possible. However, in present commercial guidance systems what is the one thing that separates the hypothetical clinical execution between the two diagrams on the right?
Quite frankly it’s the surgeon. What one individual might see as the correct trajectory for the placement of a pedicle screw or knee replacement might be different from their colleague in the next OR. In both cases robots must be accurate to the plan that has been programmed into its software by the surgeon. In addition, it should be engineered to be precise whether it is moved to a location once or numerous times.
But as we continue to innovate and build smarter surgical systems, who is determining the accuracy of the surgeon’s plan to the accuracy of a plan that provides the strongest possible clinical outcome? And what compilation of data is needed to feed a decision engine that determines the best clinical outcome?
Right now, that mental burden falls solely on the surgeon. They must pull from years of personal experience and training, a myriad of ever-changing techniques and philosophies, and the N of 1 nature of the many patients they see that do not fit the mold to do it ‘like I always do it’.
So, it begs the question can we lessen the mental burden on surgeons if robotic guidance systems had decision engines that determined the accuracy of plans to ones that would produce the best possible outcome for that patient? What if we could make them as smart as the people who designed them and the people using them?
It would still be up to the surgeon to approve the plan and insurance will never allow for such ‘improvements’ until they can garner income from it. But does this augment or detract from all surgeons go through to become experts in their field? Or, to use the cliché, does this democratize surgery?
Future forward connectivity platforms like Proximie are already allowing surgeons to share the best clinical practice in real time in a mentorship or proctoring format. In doing so it is offering even the most remote healthcare settings access to thought leaders a world away. Can we take that same collaborative reimagination of healthcare and move the decision-making assistance to a pre-operative setting in a digitized format?
Don’t get me wrong, I am not contending that surgery can become an assembly line of complex actions and movements like building cars. Every patient is different in terms of body habitus, co-morbidities, health history and so on. All must be used to make clinical decisions, but the ultimate purpose of robots is to perform actions traditionally performed by humans that are either incredibly complex, simple yet repetitive, or are performed in environments harmful to humans.
Surgical robotics and decision making
With surgical robots most often falling into the first bucket, as an industry we must feed the decision-making process with as much as we can to provide the most accurate procedure possible for the best outcome of the patient. The data collection process that this entails is massive and will require a ML engine that has immense processing power as well as real time connectivity from multiple locations.
Data flow through 5G connectivity is making this possible but the back end computational interface is still the topic of brainstorms and ‘what if’ conversations. But if we don’t start now, we delay what is possible not by months but by years and if not decades.
Some day with that engine in place, it will then be up to our teams of systems, software, mechanical, and electrical engineers to create the translation pathway of inputs to robotic end effector response that has the reproducibility and accuracy needed for our patients. How that’s done is a whole other topic for a new day best given by the talented experts working with me to realize the seemingly impossible precision and accuracy goals for our clients’ surgical systems.
And now you know why my kids will go to Alexa for their future questions! Over the past year we have looked at the challenging journey of developing robots from a programmatic perspective. This year we will start to look at the deeper questions being asked of us at CC and how we tackle those solutions together with our clients every day.
I hope this was precisely on point with our previous series and accurately struck a nerve of thought on the role of robotics in improving surgical care for all patients.
By the way, if you’re looking for the simple answer to the question What’s the difference between accuracy and precision? Accuracy and precision are both ways to quantify error. Accuracy measures how close results are to the true or known value. Precision measures how close results are to one another.